The ultimate goal of any health care screening test is early detection – to find out if people have a disease or condition before there are any outward signs of disease. Mammography is a screening test for diagnosing breast cancer. This critically essential tool enables our physicians to find breast cancer in its earliest stages, increasing the chances of successful treatment. Unfortunately, a simple online search on when to get a mammogram can turn up dozens of conflicting and confusing results.
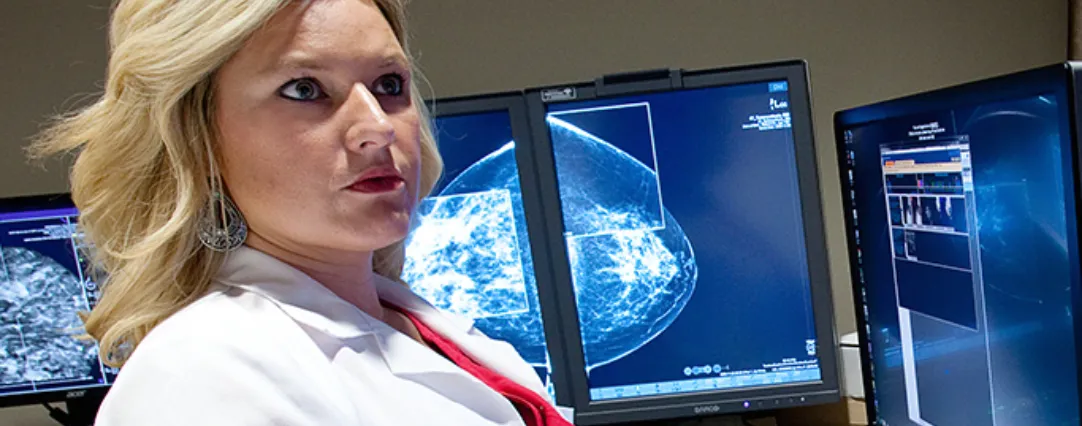
As a radiologist specializing in breast imaging, patients and other doctors often ask me about when to start annual screening mammography. I always point them to the guidelines put forth by the imaging experts: the American College of Radiology (ACR) and the Society for Breast Imaging SBI. Both have consistently recommended annual screening mammography starting at age 40 for average-risk women, and Radiology Associates of North Texas follows those recommendations.
Widely publicized recent studies and U.S. government guidelines have increased pressure to delay screening until age 45 or 50, and then, only every other year. While the push for screening mammography starting at a later age and less often would save money over time, these studies and changing guidelines are creating confusion and costing lives.
The New England Journal of Medicine (NEJM) recently published another highly questionable study, claiming extensive overdiagnosis of small tumors discovered by mammography. The study’s authors said that too many tiny, invasive cancers that normally wouldn’t need to be treated were discovered on mammograms. But that’s exactly what we want to find, because those are the cancers we can beat!
As Harvard Medical School professor of radiology and NEJM study critic Daniel Kopans, M.D., commented, “No one has ever seen a mammographically detected invasive breast cancer ‘disappear’ on its own.” The SBI said the NEJM study actually proves the opposite of what the authors intended: that mammography detects breast cancers earlier and saves lives. Kopans harshly criticized the New England Journal of Medicine for even publishing the study.
The NEJM study is flawed, and there are assumptions made that just aren’t realistic; I would tell that to any patient or any doctor that asked me. These studies make headlines in big media, online and even in medical publications, spreading confusion and fear. The result is that women don’t know what to believe, and sometimes their doctors don’t really know what to tell them either. So some women just don’t get screened, and that’s the worst of all situations.
What concerns me most overall is that government guidelines influence the Centers for Medicare and Medicaid Services (CMS), which then influences health insurance companies who make coverage decisions. The USPSTF, a panel of government experts that develops recommendations for preventive services such as mammography, currently recommends that women ages 50-74 at average risk for breast cancer undergo screening mammography every two years, with the decision to get tested younger than age 50 based on a women’s understanding of the risks versus the benefits of screening.
Government panels and studies often claim they are trying to help women avoid unnecessary testing and anxiety. In reality, they are only hurting women, because they are looking at the issue from other perspectives, not from the perspective of what saves the most lives. Ironically, the very organizations recommend- ing against annual screening mammograms until age 50 will tell you that the most life-saving benefit comes from the original recommendations put forth by the ACR, SBI and American Cancer Society: annual mammograms starting at age 40. And remember, no organization has ever come out with a recommendation against annual screening mammograms starting at age 40.
I have also heard the argument that radiologists just want to read more mammograms to make more money. Trust me: whether or not we’re reading as many mammograms, there is more than enough radiology to go around.  If federal guidelines were issued tomorrow calling for no annual mammograms until age 50, it wouldn’t change my life or my career; but it woulddrastically change things for many women, who would no longer have access to life-saving screening mammography.
If federal guidelines were issued tomorrow calling for no annual mammograms until age 50, it wouldn’t change my life or my career; but it woulddrastically change things for many women, who would no longer have access to life-saving screening mammography.
If we’re talking about what saves the most money, then start screening mammography later and end earlier. If we’re talking about what saves the most lives, there’s really not a debate. Start screening at age 40 and continue each year thereafter.
For me, and most other medical professionals that I know, the bottom line is which method saves the most lives. And there is no question that starting annual mammograms at age 40 and continuing throughout a woman’s ‘useful lifetime’ meets that standard. I say useful lifetime because a woman’s risk of breast cancer increases every year of a woman’s life, and for people to put these arbitrary numbers on when to stop is really unfair.
The end of annual screening mammography should be when a woman no longer has a healthy life ahead of her, and this was powerfully demonstrated in the study “No Evidence For Cut-Off Age for Breast Cancer Screening” presented at a recent national radiology conference in Chicago.
In the future, as personalized medicine advances, we may be able to focus in on more specific categories of women for annual screening mammograms. But my goal and my responsibility today – as a physician specialized in breast imaging – is to help save lives. If you can treat small, invasive cancers with small surgeries and not have to resort to chemotherapy, that is ideal. That’s so much better than not finding a cancer until it has developed into a much larger growth that has to be treated with major, long-term treatment plans and severely impacts a woman’s quality of life.
The next time you or someone you know is wondering, “When should I get a mammogram?” remember to check with the breast imaging experts at the American College of Radiology (acr.org) and the Society of Breast Imaging (sbi-online.org). To learn more about breast imaging and the expertise provided by our compassionate and knowledgeable breast imaging specialists, visit the Radiology Associates of North Texas Breast Imaging page.
(radntx.com/specialties/breast-imaging)
Article featured in Radiology Insights Magazine | Winter 2017
Posted: February 28, 2017