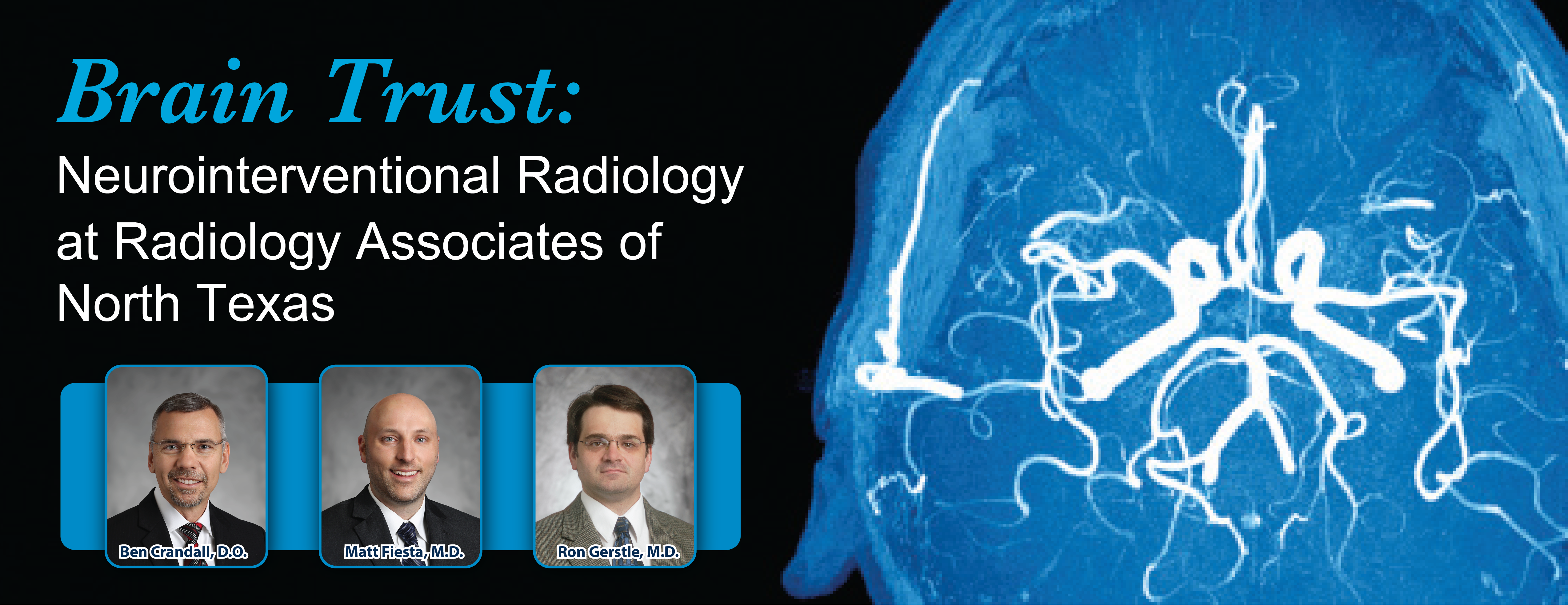
Image-guided brain plumbing: it’s a simple way to think about what interventional radiologists who work primarily with brain problems actually do. Better known as Neurointerventional Radiology, or simply “Neuro IR,” this unique subspecialty includes three of the most dedicated and passionate radiologists in the Dallas-Fort Worth region. 
The RADNTX “brain trust” includes: Ben Crandall, M.D., Matt Fiesta, M.D., and Ron Gerstle, M.D., all neurointerventional radiologists who care for patients from across the DFW Metroplex.
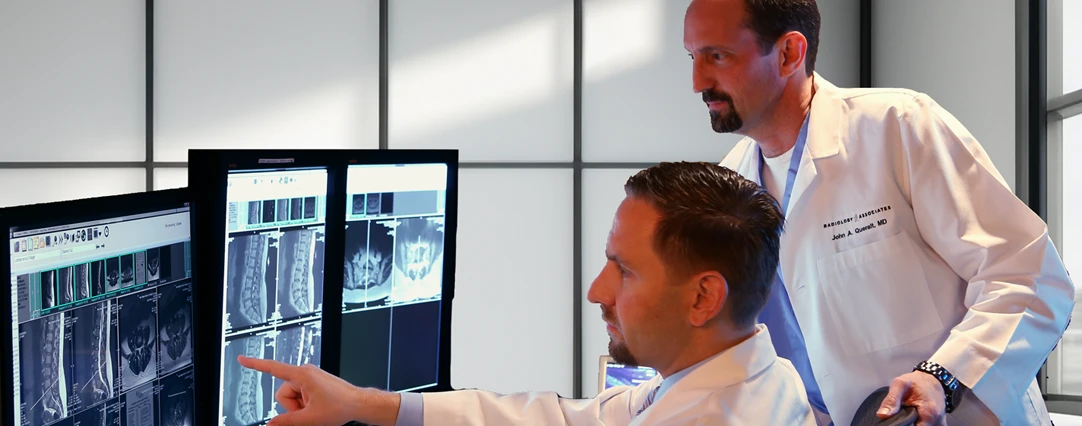
When asked about the difference between diagnostic radiologists and interventional neuroradiologists Dr. Fiesta replied, “We’re all radiologists, but as interventional neuroradiologists build on our diagnostic radiology background to interpret the image, find the problem and then act on it to treat the problem directly.”
“A diagnostic radiologist figures out what it is they are looking at and tells your doctor what they have found,” said Dr. Fiesta. “As interventional neuroradiologists, we interpret the image, but then we act on it and treat the problem directly. That’s what sets us apart.”
One of the most common but serious problems the Neuro IR team treats is intracranial (inside the brain) aneurysms – a bulging blood vessel that can break open and cause life-threatening complications. Aneurysms used to be treated with neurosurgery (brain surgery), with the neurosurgeon having to open up the skull to fix the aneurysm. Now, most aneurysms can be treated with imaging-guided, neurointerventional radiology procedures.
Using minimally invasive techniques, a neurointerventional radiologist can get to a patient’s brain through major arteries in the leg or arm to operate on and treat problems that usually involve blood vessels. Endovascular coiling, for example, can treat a brain aneurysm by blocking off the blood flow with a special metal coil, without ever having to surgically “open up” the patient.
“When you’re working inside the brain to place a coil, that’s still a form of surgery,” explained Dr. Fiesta. “But it’s minimally invasive surgery, because we use imaging to guide us from the femoral artery in the leg all the way to the where the problem is in the brain.”
“We’re working within the vessel as opposed to fixing it from the outside,” noted Dr. Gerstle. “We’re never touching anything except the inside of an artery.”
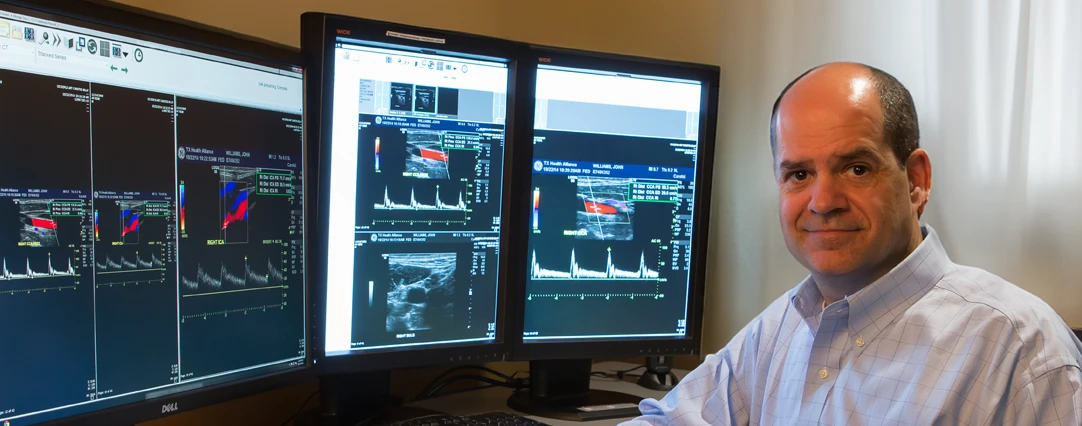
Such minimally invasive techniques are made possible through advances in medical imaging technology, which allows the radiologist to visualize the entire procedure.
“It’s all about the imaging, that’s our foundation. With those skills, we’re able to understand what we’re looking at ‘on-the-fly,’ recognize when there’s a problem and fix it quickly,” said Dr. Fiesta.
The doctors of RADNTX’ brain trust don’t normally work together and rarely even see each other because they work at different hospitals across the DFW Metroplex. However, they describe their work as collaborative, since they frequently work with other specialists.
“These are delicate, specialized procedures; you have to be very careful and aware of your limits,” said Dr. Gerstle. ”And it’s easier to be careful when you are able to talk to and collaborate with other doctors, either within your own specialty or in other specialties.”
“They might have thought of something you didn’t, and you might have thought of something they didn’t,” added Dr. Fiesta.
“It’s crucial that you coordinate with other specialties,” agreed Dr. Crandall, “so you can plot a course to the safest outcome for your patient with different specialists.”
All three talk about neurointerventional radiology as an exciting and challenging field. From its roots in the late 80’s as an offshoot of neuroradiology, Dr. Gerstle said the technology has improved tremendously over the past couple of decades.
“We’re seeing better ways to break up blood clots faster, and more efficient ways to coil an aneurysm and keep that coil in place to do its job,” said Dr. Gerstle. “We can already treat almost any aneurism interventionally. Within ten years, I predict there won’t be any aneurysm that we can’t treat.”
Visit our Radiología Neurointervencionista page for more information.
Article featured in Radiology Insights Magazine | Winter 2017
Posted: March 14, 2017